Wellness Coaching And Chronic Lung Disease

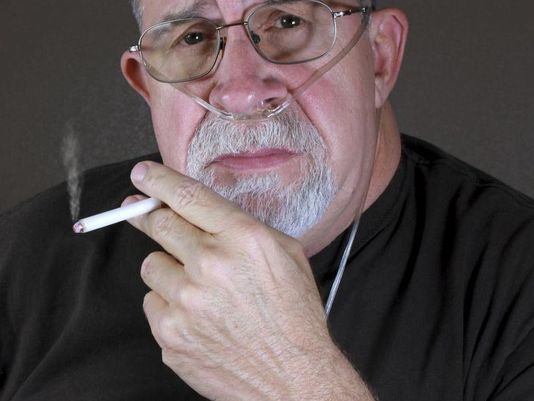
It surprises many people to discover that the third leading cause of death in the United States, behind heart disease and cancer, is chronic lower respiratory diseases. These conditions take twice as many lives annually as does diabetes. Yet, unless COPD (Chronic Obstructive Pulmonary Disease), or another such disease is part of your life or family, the seriousness of this public health challenge seems to seldom get our attention.
It’s estimated that over 15 million people in the U.S. suffer from COPD. The two main diseases that are associated with COPD are emphysema and chronic bronchitis. Approximately 22 million people in the U.S. are affected by asthma. Pneumoconiosis, also known as Black Lung Disease, is an occupational lung disease caused by inhaling coal dust. This affects more people in coal producing areas such as Appalachia and Northern Wyoming. All of these respiratory diseases have much in common, but for this article our focus will be on COPD and the ways in which lifestyle improvement can be relevant.
The most common cause of COPD is cigarette smoking and can also be related to ongoing exposure to indoor, outdoor and occupational air pollution. The preventative implications are obvious and wellness, health and safety programs can play a significant role. Like other chronic illnesses once thought to present a health challenge that we were helpless to do much about, COPD has a behavioral component that can affect the course of the illness and improve quality of life. The lifestyle medicine approach is illuminating ways in which the COPD patient can affect their condition for better or worse. Wellness and health coaching is emerging as a delivery mechanism to support COPD patients in succeeding with the lifestyle improvements that their treatment team wants to see.
 The Behavioral Side Of COPD
The Behavioral Side Of COPD
COPD normally develops slowly and is the cumulative effect of decades of exposure. Any damage that is done to the lung tissue is irreversible. There is no cure for COPD and so treatment goals aim to slow the progression of the disease and to reduce symptoms. Once properly diagnosed the most immediate behavioral interventions are environmental: (reduction in exposure to workplace or living environment pollutants, e.g. a person working in an industrial pottery who is daily exposed to clay dust); strategic: an effort to immediately cease smoking; and medically behavioral: compliance/adherence to medical treatment (e.g. bronchodilator treatments, regular medical appointments).
The overall wellness of the client is important on a number of fronts. As treatment continues, lifestyle changes, physical exercise, and regular practicing of breathing exercises may also help to improve a person’s ability to remain active, prevent exacerbations and improve one’s overall health. A good nutritious diet is very important in order to avoid infections and to keep their lungs as healthy as possible. Maintaining a healthy weight is an important factor for a person that has lung disease. If a person is overweight it can make it difficult to move around and make it even harder to breathe. Being underweight though is actually a worse prognosis than being overweight. As lung disease progresses a person will become more short of breath and fatigued. Even eating can become a lot of work and a person might find it very difficult to get all the nutrients and calories that they need.
 Improving a person’s overall strength and exercise tolerance is also a goal. The patient should speak first with their physician to determine what exercise or activities would be safe for them to do. Even though activity can make a person feel more short of breath it is vital to strengthen their muscles so that they will be able to continue to do the things they enjoy and be able to care for themselves. An individual will greatly benefit from participating consistently in a local pulmonary rehabilitation program.
Improving a person’s overall strength and exercise tolerance is also a goal. The patient should speak first with their physician to determine what exercise or activities would be safe for them to do. Even though activity can make a person feel more short of breath it is vital to strengthen their muscles so that they will be able to continue to do the things they enjoy and be able to care for themselves. An individual will greatly benefit from participating consistently in a local pulmonary rehabilitation program.
Raising self-efficacy is vital to the COPD patient. Clients/patients benefit greatly from learning as much as possible about their disease and how to manage their symptoms, work properly with their medications and make the best use of supplemental oxygen. In fact, in a study of Mindfulness training and COPD (Mindfulness: A New Approach To Reduce COPD Hospitalizations Discovery's Edge, Mayo Clinic's Online Research Magazine, Volume 8, Issue 1
http://www.mayo.edu/research/discoverys-edge/mindfulness-new-approach-reduce-copd-hospitalizations) researchers found that the patient’s perception of their disease was the greatest predictor of frequency of hospitalizations. (70% of the medical costs associated with a COPD patient come from hospitalizations).
Comorbidities
The majority of people that experience COPD also
have other chronic conditions too. Researchers aren’t sure
why, but for some reason COPD patients seem to have more
comorbid conditions than patients with other types of diseases.
In a recent study of over 1,500 people with COPD, researchers found
patients averaged having four other types of comorbid conditions whereas those that didn’t have COPD averaged less than two other
problems. This study confirmed that comorbidities are very
common in people with COPD. Some of these conditions
included heart disease, high cholesterol, high blood pressure,
diabetes, osteoporosis, arthritis, depression and cancer. These
comorbid conditions increase the likelihood of a COPD patient
being hospitalized and can also result in death (WebMD.
(2014a). COPD comorbid conditions: Heart disease, osteoporosis,
and more. Retrieved from
http://www.webmd.com/lung/copd/the-importance-of-
comorbidities.)
 Coaching And Coping
Coaching And Coping
When we review the behavioral changes that facing the challenge of COPD requires we begin to realize what a huge potential role successful lifestyle improvement has. Wellness and health coaches have been finding effective ways to assist COPD patients in their quest for a healthier life with their illness. In a cooperative study with Duke and Ohio State Universities (Coping Techniques Help Patients With COPD Improve Mentally, Physically http://psychcentral.com/news/2014/09/28/coaching-copd-patients-on-coping-helps-boost-quality-of-life/75448.html) “147 COPD patients participated in coping skills training. Psychologists provided regularly scheduled phone sessions, offering patients and their caregivers general information about COPD, step-by-step instructions in relaxation techniques such as deep breathing, tensing and releasing muscles, and ways to manage their reactions to stressful events.
Another group of 151 patients also received regular phone consultations, but only on topics such as medication and nutrition. They did not receive specific coping techniques. Participants who received training in coping skills reported improvements in their overall mental health, and lessened depression, anxiety, fatigue and shortness of breath when compared to the other group, according to the study’s findings.
Although there were no improvements in COPD-related hospitalizations or deaths, the study suggests that the low-cost approach could enhance quality of life, reduce distress and somatic symptoms, and improve physical functioning for patients, according to the researchers.” While not coaching per se, this combination of instruction and a very coach-like relationship with the psychologists who provided the phone sessions, proved the value of lifestyle improvement in increasing quality of life for COPD patients.
At the Mayo Clinic, researcher Roberto Benzo, M.D. is using Mindfulness Training (as mentioned and referenced earlier in this article) and a coach approach to not only increase client self-efficacy (and the key factor of their perception of their illness), but has shown outstanding results in reducing the number of days his subjects have needed to stay in the hospital when they are hospitalized, and reduced the overall number of needed hospitalizations.
“Patients in Dr. Benzo's clinical trials undergo an active eight-week rehabilitation program. A wellness coach uses motivational interviewing, a style of communication, to identify an appropriate exercise and develop an individualized plan. Participants are also trained to become aware of their body sensations and motions as they exercise. Active coaching is followed by monthly calls to keep them motivated.
"Daily practice is the core of the rehabilitation," Dr. Benzo says. "This means carving out a special time to be present with what is going on with their body and coming to terms with their life as it is." (http://www.mayo.edu/research/discoverys-edge/mindfulness-new-approach-reduce-copd-hospitalizations) As is found in most work with chronic illnesses, a combination of education and coaching was successful.
Dr. David Hinton Thom at the University of California, San Francisco is currently conducting a two-million dollar grant-funded study to bring the coach approach to patients in underserved communities who are challenged by COPD. “The most comprehensive disease self-management programs, i.e., "pulmonary rehabilitation," are generally not available to patients who are seen at community clinics. While self-management educational programs are more generally available, they are not often accessed by patients and do not provide personalized, sustained support. Health coaching by trained medical assistants or health workers has emerged as an effective model to provide individualized, patient-centered information, decision and self-management support, and coordination of care to improve outcomes for patients with chronic conditions. Health coaching provides patient support and reinforcement for self-management skills and activities, strategic approaches to effect behavior change, and a platform to improve comprehensiveness and quality of care. For the management of COPD, health coaches, for example, could assist patients with getting vaccinations, prescriptions, engaging in a graded exercise program, responding to exacerbations of their COPD, learning correct inhaler technique, and coordinating care between the patient's primary and specialty providers.” (Health Coaching to Reduce Disparities for Patients with Chronic Obstructive Pulmonary Disease http://www.pcori.org/research-results/2013/health-coaching-reduce-disparities-patients-chronic-obstructive-pulmonary.) Here we see how the role of a coach can become incredibly practical and strategic, assisting patients/clients with their medical self-care and self-advocacy.
 Ways Coaches Can Assist With Lifestyle Modification For COPD:
Ways Coaches Can Assist With Lifestyle Modification For COPD:
• Smoking cessation
• Securing and attending a Pulmonary Rehab Program
• Securing education about proper breathing techniques from doctor, respiratory therapist or nurse to help reduce shortness of breath, and then tracking and accountability through coaching to ensure consistent practice
• Securing education about different cough techniques and breathing positions that are more effective.
• Explore various stress management tools and relaxation techniques, learning and practicing with coaching accountability.
• Tracking the intake of water (at least 8 glasses/day), to help hydrate secretions to be able to clear them from the airway.
• Tracking, follow through and accountability re: exercising regularly to improve overall strength and cardiovascular reserve. Client should speak first with their health care provider for specific instructions.
• Assisting client with nutritional/eating goals such as:
o Eat smaller meals more frequently to diminish shortness of breath.
o Eat healthy foods and maintain a normal weight.
• Securing support for their lifestyle improvement through family, friends, workplace, and others. Coaching for connectedness.
• Securing more support through group wellness coaching and finding a greater sense of community amongst others challenged with the same illness.
The Power Of An Ally In Lifestyle Improvement
Beyond all of the concrete behavioral steps involved in lifestyle improvement nothing exceeds the importance of having a solid coaching alliance between patient, now client, and coach. Having an ally through the behavioral change process is a boost to the motivation of the client and can help them to feel that a better life is possible.
Coaches also need to be aware that clients could experience more irrational feelings and “Gremlin talk” when short of breath and oxygen level are low. Decreased oxygen levels can cause people to feel fatigued and confused, which can have a direct effect on self-efficacy. When this is suspected, once again, a referral back to the client’s treatment team is in order.
Coaches can help their clients to process the grief they feel around their loss of health. This could be directly related to diminished feelings of self-efficacy and increased helplessness. (See “Astonishing Non-compliance” in Wellness Coaching For Lasting Lifestyle Change, 2nd Ed. http://wholeperson.com/store/wellness-coaching-for-lasting-lifestyle-change.shtml) by the author.)
Facing the challenge of COPD while seeking one’s best life possible means integrating a well-coordinated treatment plan with a wellness plan focused on lasting lifestyle change. Taking the journey to one’s best health may best be done with an ally walking side-by-side with us all the way.





Only registered and logged in readers can leave comments.